Circuitry and Brain-Body Interactions | 2021
Activity and Connectivity Drive Neuronal Vulnerability and Disease Progression in Parkinson’s Disease
Study Rationale: Specific brain circuits that are highly melanized (build-up of the dark pigment neuromelanin) with age are primarily affected, particularly early, in Parkinson’s disease (PD). Models incorporating this aspect of PD have only been developed recently and show that increased neuromelanin production causes neurodegenerative changes consistent with Parkinson’s. The regulators of cellular neuromelanin metabolism have not been determined, the effect of neuromelanin on normal activity in these pathways has not been defined, the potential for neuromelanin aggregates to increase alpha-synuclein accumulation has not been evaluated, and the impact of extracellular neuromelanin on detrimental inflammatory processes has not been assessed.
Hypothesis: Activity in melanized brain circuits is a dominant factor in the initiation of PD and sustains its progression by seeding pathology in connected regions and providing the stimulus for chronic inflammation. Manipulating neuromelanin production and/or brain circuit activity can ameliorate these deficits.
Study Design: Parallel experiments will be performed in mice and non-human primates in which neuromelanin production has been induced for comparison with neuromelanin-producing neurons in people with prodromal and early Parkinson’s. To test whether activity in melanized brain circuits is a dominant factor in the initiation of PD, spatiotemporal activity mapping, imaging, and other techniques will be used, and manipulating neuromelanin production and/or brain circuit activity will be assessed as potential treatments. To determine if neurons spread PD pathology through their connectivity, seeding experiments will be performed and impacts on behavior and neurodegeneration assessed. To determine how non-neuronal mechanisms are involved in disease progression, high-resolution microscopy and cell-specific details of changes in extracellular spaces and infiltration of non-neuronal cells into the brain will be assessed.
Impact on Diagnosis: Diagnosis of neuromelanin changes in the brain are already being assessed for their diagnostic potential, but this study will determine their focus and rate of change with respect to neural activity and clinical features. Team Vila will also identify if reducing neuromelanin levels stabilizes pathology and restores brain activity.
Leadership

Lead PI (Core Leadership)
Miquel Vila, MD, PhD
Vall d'Hebron Institut de Recerca, Autonomous University of Barcelona

Co-PI (Core Leadership)
Nicola Mercuri, MD, PhD
University of Rome Tor Vergata, Fondazione Santa Lucia

Co-PI (Core Leadership)
Jose Obeso, MD, PhD
Biomedical Research Networking Center on Neurodegenerative Diseases
Project Outcomes
The project will unravel molecular mechanisms linking brain circuit activity to PD vulnerability, identify brain circuits through which PD pathology spreads across the brain and periphery, establish non-neuronal mechanisms of PD progression and determine whether modulation of neuromelanin levels and/or brain circuit activity can restore PD circuit dysfunction & pathology. View Team Outcomes.
Team Outputs
Click the following icons to learn more about the team’s outputs:
Overall Contributions
Here is an overview of how this team’s article findings have contributed to the PD field as of May 2025. There are two different categorizations of these contributions – one by impact to the PD community and a second by scientific category.
Impact
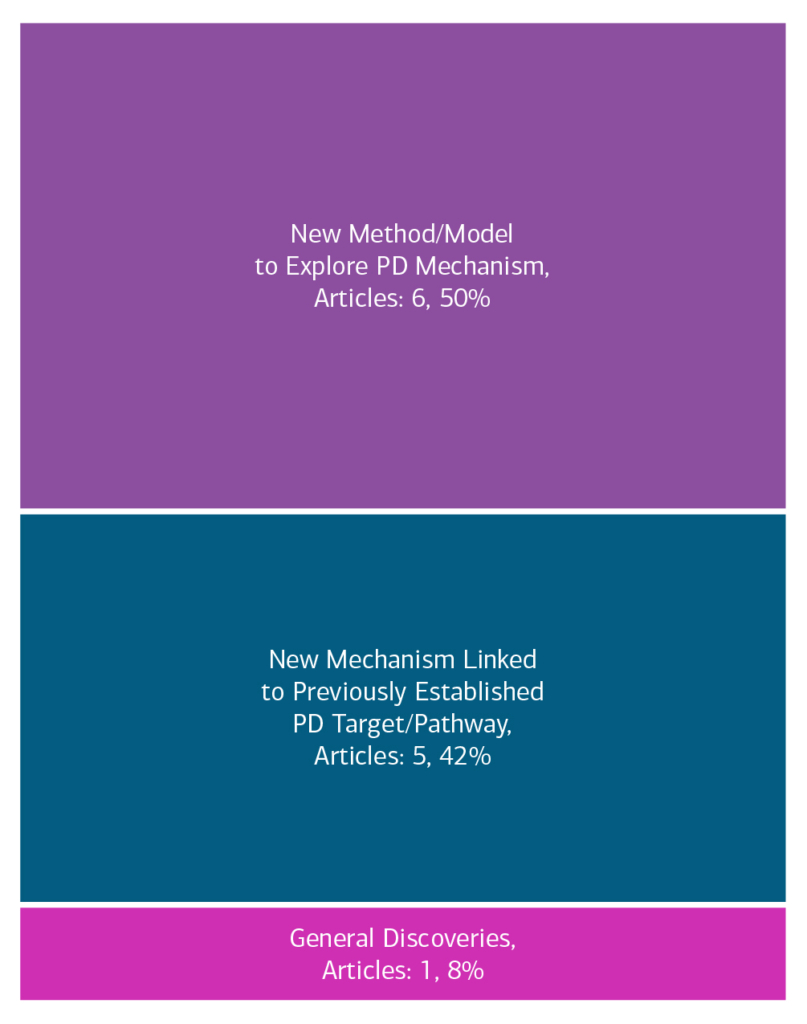
Category

Featured Output
Below is an example of a research output from the team that contributes to the ASAP mission of accelerating discoveries for PD.
Sex-dimorphic effects of neuromelanin buildup in rodent nigral dopamine neurons: implications for sex-biased vulnerability in Parkinson’s disease
This paper evaluates sex-specific alterations in neuromelanin. This may shed light on some aspects of sexual dimorphism in human PD.
Team Accolades
Members of the team have been recognized for their contributions.
- Network Spotlights: Yuhong Fu, Ka Wai Lee
- Awards
- 2023 Collaborative Meeting: 2023 Collaborative Meeting: Julia Chocarro (Data Blitz Talk Award Winner; London)

Other Team Activities
- Working Groups:
- ANALYSE Neuropathology – Glenda Halliday (Co-Chair)
In the News
- Research project coordinated by Vall d’Hebron receives $11M to study Parkinson’s disease (Vall d’Hebron, October 25, 2021)
- Researchers from ACHUCARRO part of new 11 million dollars consortium to tackle Parkinson’s disease (ACHUCARRO, October 26, 2021)